- 首页 > 正文
ERA大咖谈丨Ⅲ期VALIANT试验52周数据揭晓:加速补体抑制疗法革新
发表时间:2025-08-19 14:57:57
编者按:在第62届欧洲肾脏协会(ERA)年会上,瑞士洛桑大学附属医院(CHUV)肾脏病学教授Fadi Fakhouri博士聚焦补体抑制疗法及其在C3肾小球病(C3G)和原发性免疫复合物膜增生性肾小球肾炎(IC-MPGN)中的应用进行学术报告,揭示了临床需要多种补体抑制剂的核心逻辑,并分享了Pegcetacoplan治疗C3G和原发性(特发性)IC-MPGN的Ⅲ期VALIANT试验的52周结果详细数据。肾医线就此话题对Fadi Fakhouri博士进行了专访,本文整理Fadi Fakhouri博士的大会报告及采访的主要内容,与广大肾脏病医生共享。
一、补体系统复杂性驱动多样化治疗需求
“补体系统包含40余种蛋白质,通过经典、凝集素和替代三条途径激活,不同肾脏疾病中补体的致病机制差异显著。”Fakhouri指出,“炎症性损伤多由C5激活介导,而C3G的关键驱动因素是C3沉积”。这种机制异质性要求治疗必须“精准靶向”——例如针对替代途径失调的C3G,需特异性抑制C3转化酶,而炎症为主的疾病则需靶向C5。此外,同一患者在疾病不同阶段的补体活化模式可能动态变化,进一步凸显了多样化抑制剂的必要性。
他以图表展示补体系统级联反应(图1):经典途径从C1复合物启动,替代途径依赖C3b与B因子结合,而终末途径共同形成膜攻击复合物(MAC)。“就像交响乐团需要不同乐器协作,补体系统的精密平衡一旦打破,就需要不同‘调节器’来纠正。”他强调,这种复杂性也体现在临床——约50%~80%的C3G患者存在C3肾炎因子,4%~12%携带抗H因子抗体(Kidney Int. 2020 Nov;98(5):1135-1148.),不同抗体亚型对应不同的治疗靶点。
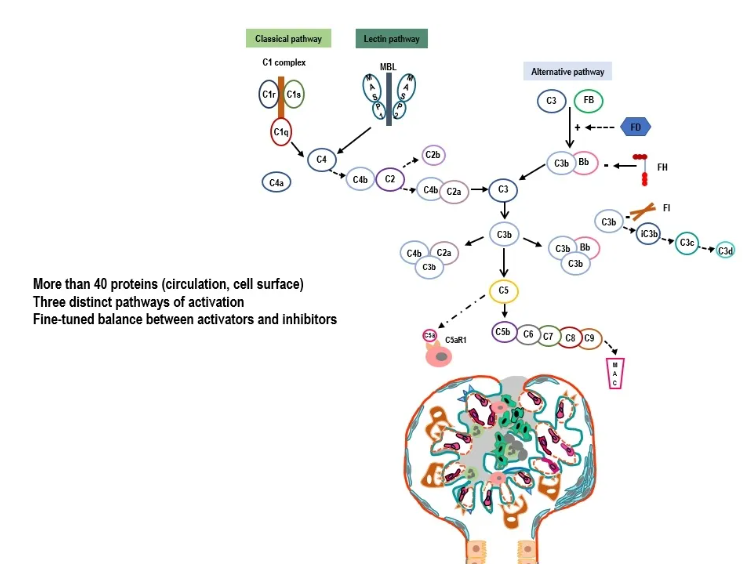
图1. 复杂的补体系统
Nephrology On-line: Your presentations highlight the evolving role of complement inhibition in treating C3G and primary IC-MPGN. Could you explain why multiple different complement inhibitors are needed in clinical practice?
Dr Fakhouri: As you know, the complement system is very complex, and even the involvement of complement in different kidney diseases relies on different molecules in the complement system. So, we need different therapeutic targets. For example, inflammation is more mediated by C5 activation. Whereas in C3G, the main driver is C3 deposition. So, you have different mechanisms of injury to the kidney due to complement, and we need to target each one specifically depending on the context of the disease, even sometimes, depending on the course of the disease, over time in a single patient.
二、VALIANT试验:补体抑制的长期疗效验证
针对Pegcetacoplan(培西他普)的Ⅲ期VALIANT试验数据成为本次报告的焦点。该试验为随机前瞻性试验,旨在评估Pegcetacoplan在青少年和成人C3G及免疫复合物性疾病患者中的疗效,共纳入124例患者。
在报告中,Fakhouri教授展示了治疗前后的肾活检对比:基线时弥漫性C3c阳性的肾小球,在26周的Pegcetacoplan治疗后转为阴性。机制上,该药物通过抑制C3转化酶,阻断C3b生成及下游炎症级联,从而减少肾小球损伤。试验还证实,治疗26周时,无论患者年龄(12岁以上)、疾病类型(C3G或IC-MPGN)、移植状态或基线蛋白尿水平,疗效均一致。例如,基线蛋白尿≥3 g/g的患者治疗后蛋白尿减少72.1%,合并免疫抑制剂治疗的患者也获得70.3%的降幅。
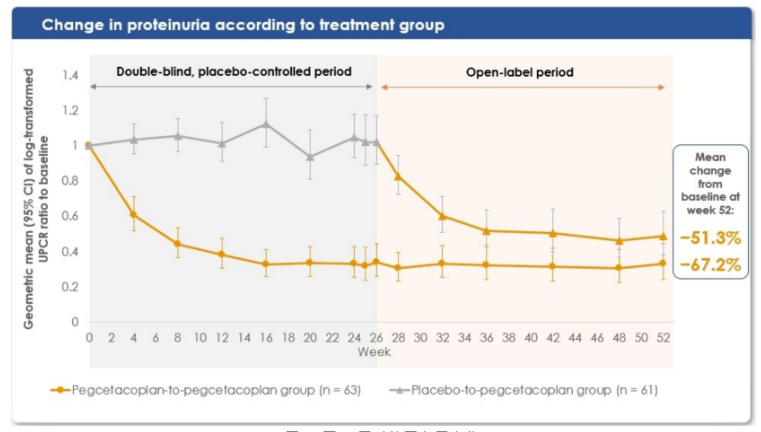
治疗52周(1年)时的结果显示,无论是初始即接受治疗还是6个月后从安慰剂转用Pegcetacoplan的患者,蛋白尿分别减少51%和67%(图2)——这种降幅在肾小球疾病中极为罕见。更值得关注的是,71%的患者在26周重复肾活检中显示C3c沉积完全清除,“传统治疗中,C3沉积的逆转几乎难以想象。”C3c 沉积的逆转是C3G和IC-MPGN患者疗效的关键标志。
此外,估算肾小球滤过率(eGFR)在一年内保持稳定。安慰剂组在初始六个月内 eGFR 有下降趋势,但转为Pegcetacoplan治疗后,肾功能有所恢复,最终 eGFR 与初始即接受治疗的患者相似。基于蛋白尿减少、肾脏C3c清除和 eGFR 早期稳定,VALIANT试验的这些结果令人瞩目。
图片
图2. 至52周时的蛋白尿变化
安全性方面,药物相关不良事件多为轻度输液反应,未出现脑膜炎球菌感染等严重并发症,长期使用的安全性与短期数据一致。这为临床提供了重要参考:Pegcetacoplan不仅疗效显著,且可避免糖皮质激素的副作用,尤其适用于需长期治疗的患者。
Nephrology On-line: The VALIANT trial with pegcetacoplan has shown sustained efficacy over 52 weeks in patients with C3G and IC-MPGN. What are the key clinical implications of these results for patients and clinicians?
Dr Fakhouri: The VALIANT study was a randomized prospective trial assessing the efficacy of pegcetacoplan in C3 glomerulopathy (C3G) and immune complex in adolescent and adult patients. After six months, all the placebo group was switched to pegcetacoplan. Here, we present the data at 52 weeks, one year, that are impressive. To make it simple for you, I'm going to give you just three figures – 51-67%0% reduction in proteinuria in patients who were from the beginning on pegcetacoplan and patients switched from placebo to pegcetacoplan, respectively; Such reduction in proteinuria is rarely seen in glomerular diseases. Besides, 71% of patients clearing all their C3c deposits in the kidney at a repeat kidney biopsy at 26 weeks (which is in my point of view a very impressive finding, because we are not very accustomed to seeing that);. The reversal of C3c deposits is a key finding of efficacy in C3G patients and immune complex-mediated membranoproliferative glomerulonephritis (IC-MPGN) patients. The short finding is that you have a stabilization of eGFR over one year. The placebo group tended to decrease in the initial six months, and then when they were switched to pegcetacoplan, they regained some renal function and, at the end, the eGFR was similar to those patients treated from the beginning with pegcetacoplan. Very impressive results based on proteinuria reduction, C3c removal from the kidney, and stabilization of eGFR as early as one year.
Fakhouri教授指出:“当前,我们正处于快速变革的时代,补体抑制剂将在不同适应证中找到定位。”面对补体介导性肾病的治疗前景,Fakhouri教授勾勒出清晰的发展蓝图:
抗炎药物的迭代升级:C5抑制剂有望取代糖皮质激素,成为炎症性肾病的一线选择。“患者可以告别激素导致的骨质疏松、感染风险,同时获得更持久的肾脏缓解。”
精准靶向治疗的普及:从“一刀切”的全身性抑制转向精准调控。例如,替代途径异常的C3G患者可靶向C3转化酶,而经典途径激活为主的疾病则需抑制C1复合物。这种“病理机制导向”的治疗模式将大幅提升疗效。
可及性与成本优化:随着更多企业入局补体领域以及更多补体药物上市,药物价格有望下降。竞争将推动技术创新,促进药物价格下降,使全球患者有能力负担并获得治疗。
Nephrology On-line: How do you envision the treatment paradigm for complement-mediated kidney diseases evolving in the next 5 to 10 years, and what research questions are most urgent to address?
Dr Fakhouri: This is a very excellent question, because I think we are living in very changing, moving times and complement inhibitors will find their place in different indications. For example, I see in the future that C5 inhibitors will replace corticosteroids sooner or later as anti-inflammatory drugs in inflammatory kidney disease. This would be a great change for doctors, but especially for patients. They could be spared the side effects of corticosteroids while achieving potentially a better renal remission. The second change I see is that we are moving towards a more targeted, specific pathogenesis-based approach to disease, where if you have an alternative pathway dysregulated, you have to target the alternative pathway. So, we are moving towards a fine-tuned, precise inhibition of the complement system, not a global inhibition like we had initially with C5 inhibition. And the third trend I see is a decrease in price due to the increase in the number of drugs and companies involved in the complement field, which would be good news for patients because decrease in price would make it more affordable and more easily available for patients worldwide.
四、补体领域:下一个肾脏病学革新前沿
“两三年前,SGLT2抑制剂和GLP-1受体激动剂引领了代谢性肾病的突破;如今,补体抑制正在开启新的治疗纪元。”Fakhouri在访谈中感慨。在ERA年会的众多议题中,补体抑制专场无疑成为焦点。从基础研究到临床转化的加速,将让补体靶向治疗成为继免疫抑制剂之后的又一里程碑。
Nephrology On-line: You have probably given a lot of talks, also joined a lot of sessions. Have you seen any sessions that you think are particularly interesting?
Dr Fakhouri: I think the complement inhibition is making a great revolution. Two or three years ago, we had the SGLT2 inhibitors and GLP-1 receptor agonists emerging into the light, and now it is time for complement inhibition. That is why I'm very happy to be here.
总结及展望
肾脏疾病治疗的范式正发生重要变革,尤其是补体治疗领域。除Pegcetacoplan外,针对C5、C1q、H因子等靶点的抑制剂已进入不同研发阶段,形成覆盖补体全通路的治疗矩阵。这不是单一药物的胜利,而是整个领域对疾病机制深入理解的成果。随着精准医学和人工智能在生物标志物发现中的应用,补体抑制疗法将进一步个性化,为终末期肾病的预防带来希望。
未来肾脏疾病的诊断不仅要依赖肾活检,更要结合血液和尿液中的补体活化标志物,如 C3a、C5a,实现疗效的动态监测。” 此外,如何确定最佳治疗疗程、筛选能安全停药的患者,以及探索补体抑制剂与其他靶向药物的联合方案,都是亟待解决的课题。
一、补体系统复杂性驱动多样化治疗需求
“补体系统包含40余种蛋白质,通过经典、凝集素和替代三条途径激活,不同肾脏疾病中补体的致病机制差异显著。”Fakhouri指出,“炎症性损伤多由C5激活介导,而C3G的关键驱动因素是C3沉积”。这种机制异质性要求治疗必须“精准靶向”——例如针对替代途径失调的C3G,需特异性抑制C3转化酶,而炎症为主的疾病则需靶向C5。此外,同一患者在疾病不同阶段的补体活化模式可能动态变化,进一步凸显了多样化抑制剂的必要性。
他以图表展示补体系统级联反应(图1):经典途径从C1复合物启动,替代途径依赖C3b与B因子结合,而终末途径共同形成膜攻击复合物(MAC)。“就像交响乐团需要不同乐器协作,补体系统的精密平衡一旦打破,就需要不同‘调节器’来纠正。”他强调,这种复杂性也体现在临床——约50%~80%的C3G患者存在C3肾炎因子,4%~12%携带抗H因子抗体(Kidney Int. 2020 Nov;98(5):1135-1148.),不同抗体亚型对应不同的治疗靶点。
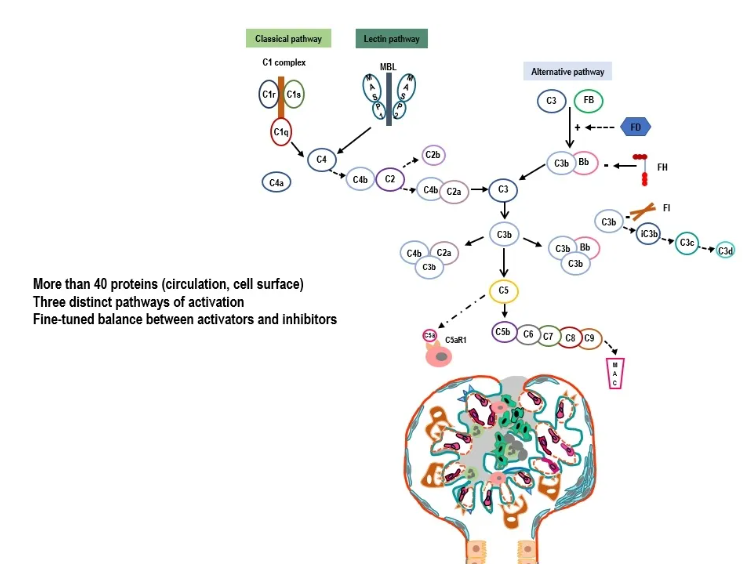
图1. 复杂的补体系统
Nephrology On-line: Your presentations highlight the evolving role of complement inhibition in treating C3G and primary IC-MPGN. Could you explain why multiple different complement inhibitors are needed in clinical practice?
Dr Fakhouri: As you know, the complement system is very complex, and even the involvement of complement in different kidney diseases relies on different molecules in the complement system. So, we need different therapeutic targets. For example, inflammation is more mediated by C5 activation. Whereas in C3G, the main driver is C3 deposition. So, you have different mechanisms of injury to the kidney due to complement, and we need to target each one specifically depending on the context of the disease, even sometimes, depending on the course of the disease, over time in a single patient.
二、VALIANT试验:补体抑制的长期疗效验证
针对Pegcetacoplan(培西他普)的Ⅲ期VALIANT试验数据成为本次报告的焦点。该试验为随机前瞻性试验,旨在评估Pegcetacoplan在青少年和成人C3G及免疫复合物性疾病患者中的疗效,共纳入124例患者。
在报告中,Fakhouri教授展示了治疗前后的肾活检对比:基线时弥漫性C3c阳性的肾小球,在26周的Pegcetacoplan治疗后转为阴性。机制上,该药物通过抑制C3转化酶,阻断C3b生成及下游炎症级联,从而减少肾小球损伤。试验还证实,治疗26周时,无论患者年龄(12岁以上)、疾病类型(C3G或IC-MPGN)、移植状态或基线蛋白尿水平,疗效均一致。例如,基线蛋白尿≥3 g/g的患者治疗后蛋白尿减少72.1%,合并免疫抑制剂治疗的患者也获得70.3%的降幅。
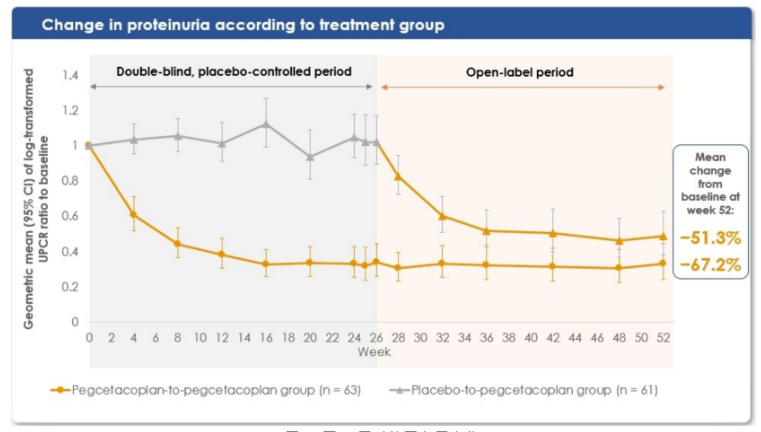
治疗52周(1年)时的结果显示,无论是初始即接受治疗还是6个月后从安慰剂转用Pegcetacoplan的患者,蛋白尿分别减少51%和67%(图2)——这种降幅在肾小球疾病中极为罕见。更值得关注的是,71%的患者在26周重复肾活检中显示C3c沉积完全清除,“传统治疗中,C3沉积的逆转几乎难以想象。”C3c 沉积的逆转是C3G和IC-MPGN患者疗效的关键标志。
此外,估算肾小球滤过率(eGFR)在一年内保持稳定。安慰剂组在初始六个月内 eGFR 有下降趋势,但转为Pegcetacoplan治疗后,肾功能有所恢复,最终 eGFR 与初始即接受治疗的患者相似。基于蛋白尿减少、肾脏C3c清除和 eGFR 早期稳定,VALIANT试验的这些结果令人瞩目。
图片
图2. 至52周时的蛋白尿变化
安全性方面,药物相关不良事件多为轻度输液反应,未出现脑膜炎球菌感染等严重并发症,长期使用的安全性与短期数据一致。这为临床提供了重要参考:Pegcetacoplan不仅疗效显著,且可避免糖皮质激素的副作用,尤其适用于需长期治疗的患者。
Nephrology On-line: The VALIANT trial with pegcetacoplan has shown sustained efficacy over 52 weeks in patients with C3G and IC-MPGN. What are the key clinical implications of these results for patients and clinicians?
Dr Fakhouri: The VALIANT study was a randomized prospective trial assessing the efficacy of pegcetacoplan in C3 glomerulopathy (C3G) and immune complex in adolescent and adult patients. After six months, all the placebo group was switched to pegcetacoplan. Here, we present the data at 52 weeks, one year, that are impressive. To make it simple for you, I'm going to give you just three figures – 51-67%0% reduction in proteinuria in patients who were from the beginning on pegcetacoplan and patients switched from placebo to pegcetacoplan, respectively; Such reduction in proteinuria is rarely seen in glomerular diseases. Besides, 71% of patients clearing all their C3c deposits in the kidney at a repeat kidney biopsy at 26 weeks (which is in my point of view a very impressive finding, because we are not very accustomed to seeing that);. The reversal of C3c deposits is a key finding of efficacy in C3G patients and immune complex-mediated membranoproliferative glomerulonephritis (IC-MPGN) patients. The short finding is that you have a stabilization of eGFR over one year. The placebo group tended to decrease in the initial six months, and then when they were switched to pegcetacoplan, they regained some renal function and, at the end, the eGFR was similar to those patients treated from the beginning with pegcetacoplan. Very impressive results based on proteinuria reduction, C3c removal from the kidney, and stabilization of eGFR as early as one year.
Fakhouri教授指出:“当前,我们正处于快速变革的时代,补体抑制剂将在不同适应证中找到定位。”面对补体介导性肾病的治疗前景,Fakhouri教授勾勒出清晰的发展蓝图:
抗炎药物的迭代升级:C5抑制剂有望取代糖皮质激素,成为炎症性肾病的一线选择。“患者可以告别激素导致的骨质疏松、感染风险,同时获得更持久的肾脏缓解。”
精准靶向治疗的普及:从“一刀切”的全身性抑制转向精准调控。例如,替代途径异常的C3G患者可靶向C3转化酶,而经典途径激活为主的疾病则需抑制C1复合物。这种“病理机制导向”的治疗模式将大幅提升疗效。
可及性与成本优化:随着更多企业入局补体领域以及更多补体药物上市,药物价格有望下降。竞争将推动技术创新,促进药物价格下降,使全球患者有能力负担并获得治疗。
Nephrology On-line: How do you envision the treatment paradigm for complement-mediated kidney diseases evolving in the next 5 to 10 years, and what research questions are most urgent to address?
Dr Fakhouri: This is a very excellent question, because I think we are living in very changing, moving times and complement inhibitors will find their place in different indications. For example, I see in the future that C5 inhibitors will replace corticosteroids sooner or later as anti-inflammatory drugs in inflammatory kidney disease. This would be a great change for doctors, but especially for patients. They could be spared the side effects of corticosteroids while achieving potentially a better renal remission. The second change I see is that we are moving towards a more targeted, specific pathogenesis-based approach to disease, where if you have an alternative pathway dysregulated, you have to target the alternative pathway. So, we are moving towards a fine-tuned, precise inhibition of the complement system, not a global inhibition like we had initially with C5 inhibition. And the third trend I see is a decrease in price due to the increase in the number of drugs and companies involved in the complement field, which would be good news for patients because decrease in price would make it more affordable and more easily available for patients worldwide.
四、补体领域:下一个肾脏病学革新前沿
“两三年前,SGLT2抑制剂和GLP-1受体激动剂引领了代谢性肾病的突破;如今,补体抑制正在开启新的治疗纪元。”Fakhouri在访谈中感慨。在ERA年会的众多议题中,补体抑制专场无疑成为焦点。从基础研究到临床转化的加速,将让补体靶向治疗成为继免疫抑制剂之后的又一里程碑。
Nephrology On-line: You have probably given a lot of talks, also joined a lot of sessions. Have you seen any sessions that you think are particularly interesting?
Dr Fakhouri: I think the complement inhibition is making a great revolution. Two or three years ago, we had the SGLT2 inhibitors and GLP-1 receptor agonists emerging into the light, and now it is time for complement inhibition. That is why I'm very happy to be here.
总结及展望
肾脏疾病治疗的范式正发生重要变革,尤其是补体治疗领域。除Pegcetacoplan外,针对C5、C1q、H因子等靶点的抑制剂已进入不同研发阶段,形成覆盖补体全通路的治疗矩阵。这不是单一药物的胜利,而是整个领域对疾病机制深入理解的成果。随着精准医学和人工智能在生物标志物发现中的应用,补体抑制疗法将进一步个性化,为终末期肾病的预防带来希望。
未来肾脏疾病的诊断不仅要依赖肾活检,更要结合血液和尿液中的补体活化标志物,如 C3a、C5a,实现疗效的动态监测。” 此外,如何确定最佳治疗疗程、筛选能安全停药的患者,以及探索补体抑制剂与其他靶向药物的联合方案,都是亟待解决的课题。
- 推荐文章
肾识百科|“狼”疮妈妈的“孕”筹帷幄:7问7答囊括狼疮肾炎与妊娠的那些事儿
肾例明鉴|高复发率、复杂性,让肾脏科医师头疼!一例难治性微小病变肾病诊治经验分享
新型质谱技术显著提升PLA2R阴性MN的抗原检出率,为MN的精准诊断、病因探寻及个体化治疗提供坚实技术支撑
重磅丨泰它西普在中国IgA肾病Ⅲ期临床研究中取得突破性进展
儿童罕见肾脏病——让孩子年轻轻轻就得肾结石,元凶多是这种肾脏遗传病
房中则教授:肠道菌群——代谢性疾病防治的新靶点与新策略
最新资讯|全球首个膜性肾病特异性治疗药物Felzartamab的Ⅲ期临床试验PROMINENT正式启动
尿液KIM-1、MCP-1及EGF可作为糖尿病肾病进展的独立预测因子:基于CRIC研究的病例队列分析
CSE 2025 | 洪天配教授:GLP-1受体激动剂对胰岛β细胞的影响:改善功能还是延缓衰竭?
CNA2025|张爱华教授:运动因子在CKD血管钙化调控中的作用机制探讨
诺锐达®(盐酸阿曲生坦片)在中国获批IgA肾病适应证,成为国内首个针对该疾病的非免疫性疗法
9.9%白蛋白尿进展,32.5%肾功能恶化!北京医院郭立新、潘琦教授团队揭示T2DM患者DKD进展轨迹
重新构想SGLT2i:拓展其在心血管-肾脏-代谢及更多领域的新用途
CNA 2025 | IgA肾病治疗策略迎革命性转变,APRIL抑制剂——斯贝利单抗成开路先锋
陈孟华教授:腹膜透析患者营养不良的评估与管理
肾例明鉴 | 原发性干燥综合征合并冷球蛋白血症性肾小球肾炎伴非弥漫性膜增生性肾小球肾炎样病变一例
血清阴性≠排除狼疮肾炎!一例特殊病例的诊断与治疗突破 图片 点击蓝字 关注我们
"磷"危时刻——李贵森教授带你了解透析患者高磷血症管理策略与临床新进展
TESTING研究事后分析:激素治疗可改善高进展风险IgA肾病的肾脏结局,无论基线蛋白尿或eGFR如何
ACC/AHA等十余家学术机构联合发布新高血压指南,强调预防、尽早治疗以降低心血管疾病风险
CKD患者血压管理的破局之道——许钟镐教授详解临床“秘籍”
肾域华章 | 上海曙光医院课题组揭示中药复方仙黄方抗肾间质纤维化的分子机制!
病例分享 | 两大“健康杀手”协同攻击,如何打破心肾恶性循环?一例4型心肾综合征的诊治启示
破局“肾”痒!思舒静®(安瑞克芬注射液)Ⅲ期数据登顶国际顶刊《BMJ》!
从CKM到CLKM——郑明华/周晓东教授nature reviews:cardiology发文,呼吁将肝脏正式纳入整合管理框架
醛固酮靶向治疗:在难治性高血压与慢性肾脏病中实现早期干预的新范式
非奈利酮用于CKD合并T2DM治疗的作用机制和循证回顾
指南共识 | 2025肾脏移植受者术后切口并发症临床诊疗指南,14大临床问题28条解决方案!
肾研药讯丨FDA批准两款蔗糖铁注射液仿制药用于慢性肾脏病相关缺铁性贫血治疗
CNA2025|赵建荣教授:IgA肾病中西医结合治疗的现状、机制与发展方向
CNA2025|魏佳莉教授:继发性IgA肾病九大病因解析
CNA2025|周晓玲教授:乙肝相关性肾炎诊治进展
肾例明鉴|警惕,这个病毒近期高发!流感季里肆虐的甲流,让不少人的肾脏不堪重负
关于GLP-1RA的最大误解:心肾获益来源于减重?
靶向炎症和纤维化:T2DM相关CKD患者早期优化治疗策略
儿童、成人、老人,谁的肾脏在狼疮肾炎中更“扛造”?数据告诉你真相
征文投稿倒计时30天 | 中华医学会肾脏病学分会第二十八届学术年会
CNA2025|丁峰教授:从尿毒症毒素看充分性血液透析的前沿策略
KI杂志重磅公布:eGFR急性下降很慌?FIDELITY汇总分析证实非奈利酮的心肾获益根本不受它的影响
病例分享 | 年轻女性突发恶性高血压,警惕沉默的血压“操控者”——肾动脉纤维肌性发育不良
CNA2025|许冬梅教授:膜性肾病发病机制研究进展
CKJ重磅公布:内皮素受体拮抗剂首个荟萃分析证实其显著降低IgA肾病患者蛋白尿、血压
关于举办2025年肾脏病研究进展南方论坛暨医疗大数据论坛的通知
ERA发布IgAN突破性疗法:斯贝利单抗III期中期分析结果振奋人心,IgAN患者uPCR-24h显著降低51.2%
CKJ丨系统性红斑狼疮肾炎(LN)管理的十大建议
JAMA公布Launch-HTN临床试验结果:醛固酮合成酶抑制剂治疗高血压
CNA2025|涂晓文教授:中晚期糖尿病肾脏疾病临床关注问题解析
医生,我周末才运动,行吗?一项基于5万余例糖尿病患者的研究给出肯定答案!
CNA2025|陈香美院士开幕引航,开启肾病防治数智新征程
从机制到临床:一文读懂非奈利酮在CKM综合征中的最新证据
肾例明鉴丨男子烫伤后肾损伤严重,肾脏竟出现100%新月体,为何让医生直呼意想不到?
狼疮肾炎还是继发性膜性肾病?从诊断困境到乙肝相关性肾炎治疗新进展
征文通知 | 中华医学会肾脏病学分会第二十八届学术年会
RNA疗法在肾脏疾病中的应用前景与现状
Zigakibart在IgA肾病治疗中的临床价值:基于Ⅰ/Ⅱ期研究的多维度分析
